Before we get into this post about how to write nursing diagnosis, it is best to cover definitions of nursing diagnosis and medical diagnosis. While these two terms seem similar, they are in fact not the same and require different approaches when writing or assessing them.
Nursing diagnosis forms the basis of the nursing process. As such, it is an integral part of clinical practice and medical care. Nursing diagnosis provides a framework to direct and focus nursing care and to plan and assess the outcomes of the care given. The nurse uses clinical judgment to make decisions about each patient. Clinical judgment is based on knowledge, experience, and other factors such as the assessment data, the available diagnostic information, and the characterization of the patient’s health status at that particular time.
Table of Contents
What is a nursing diagnosis?
A nursing diagnosis is a clinical judgment concerning human response to health conditions/life processes, or vulnerability for that response, by an individual, family, group, or community. A nursing diagnosis provides the basis for the selection of nursing interventions to achieve outcomes for which the nurse has accountability. Nursing diagnoses are developed based on data obtained during the nursing assessment and enable the nurse to develop the care plan. Medical and nursing diagnoses have different goals: a medical diagnosis identifies a variation from a norm, while a nursing diagnosis should judge the existence of a potential for enhancing self-care.
Purposes of Nursing Diagnosis
The purpose of the nursing diagnosis is as follows:
- Helps identify nursing priorities and help direct nursing interventions based on identified priorities.
- Helps the formulation of expected outcomes for quality assurance requirements of third-party payers.
- Nursing diagnoses help identify how a client or group responds to actual or potential health and life processes and knowing their available resources of strengths that can be drawn upon to prevent or resolve problems.
- Provides a common language and forms a basis for communication and understanding between nursing professionals and the healthcare team.
- Provides a basis of evaluation to determine if nursing care was beneficial to the client and cost-effective.
- For nursing students, nursing diagnoses are an effective teaching tool to help sharpen their problem-solving and critical thinking skills.
Difference between Medical and Nursing Diagnoses
The term nursing diagnosis is associated with three different concepts. It may refer to the distinct second step in the nursing process, diagnosis. Also, nursing diagnosis applies to the label when nurses assign meaning to collected data appropriately labeled with NANDA-I-approved nursing diagnosis. For example, during the assessment, the nurse may recognize that the client is feeling anxious, fearful, and finds it difficult to sleep. It is those problems which are labeled with nursing diagnoses: respectively, Anxiety, Fear, and Disturbed Sleep Pattern. Lastly, a nursing diagnosis refers to one of many diagnoses in the classification system established and approved by NANDA. In this context, a nursing diagnosis is based upon the response of the patient to the medical condition. It is called a ‘nursing diagnosis’ because these are matters that hold a distinct and precise action that is associated with what nurses have autonomy to take action about with a specific disease or condition. This includes anything that is a physical, mental, and spiritual type of response. Hence, a nursing diagnosis is focused on care.
Comparison of Nursing and Medical Diagnoses
Nursing diagnoses vs medical diagnoses
A medical diagnosis, on the other hand, is made by the physician or advance health care practitioner that deals more with the disease, medical condition, or pathological state only a practitioner can treat. Moreover, through experience and know-how, the specific and precise clinical entity that might be the possible cause of the illness will then be undertaken by the doctor, therefore, providing the proper medication that would cure the illness. Examples of medical diagnoses are Diabetes Mellitus, Tuberculosis, Amputation, Hepatitis, and Chronic Kidney Disease. The medical diagnosis normally does not change. Nurses are required to follow the physician’s orders and carry out prescribed treatments and therapies.
As explained above, now it is easier to distinguish nursing diagnosis from that of a medical diagnosis. Nursing diagnosis is directed towards the patient and his physiological and psychological response. A medical diagnosis, on the other hand, is particular with the disease or medical condition. Its center is on the illness.
How to Write Nursing Diagnosis
Part 1: Collecting and Analyzing Data
- Observe the patient’s symptoms. Take note of the patient’s injuries or symptoms of their condition. Formulate a basic description of the problem the patient seems to be having, based on the signs and symptoms you see.[3]
- For example, if you have a patient who was diagnosed with a traumatic brain injury, they may seem confused and disoriented. You could write down that they don’t seem to understand where they are, or why they are in the hospital.
- Don’t worry about using official terminology at this point. You can “translate” your observations later. Focus on getting down what you see in your own words.
- Talk to the patient and their loved ones about how they’re feeling. Your actual nursing diagnosis includes information from the patient as well as those around them. Family members and friends can provide details about changes in the patient’s behavior and appearance. They can also tell you how the patient’s condition is affecting them.[4]
- Ask the patient questions to better understand their response to their condition and how they are coping with various symptoms. For example, if you have a patient who was diagnosed with a traumatic brain injury, you might ask if they know where they are or why they’re there. You also might ask them what day it is, or who the president is, to get a better understanding of their connection to reality.
- The response and attitude of friends and family may also impact the patient’s problems. For example, if the patient’s spouse is stressed out or anxious, they may increase the patient’s anxiety.Possible Questions to AskWhat makes the symptom better or worse?
What have you done to get relief?
How would you characterize the symptom?
How does the symptom rate on a severity scale of 1 to 10?
When did the symptom start? Is the onset sudden or gradual?
How long does the symptom last?
- Evaluate the patient’s response to their symptoms. Look at what the patient has done to alleviate their symptoms and how they are coping with any pain or loss of functioning. Consider the patient’s attitude and their treatment of people around them, including loved ones and health care providers.[5]
- For example, if the patient is defiant and lashes out at loved ones or at health care providers, they may be in a lot of pain or have high levels of anxiety.
- Distinguish between objective and subjective data. Subjective data is what the patient tells you about how they feel. It’s their perception, and can’t be verified. Objective data, on the other hand, comes from observations that are measurable and verifiable using scientific methods.[6]
- Data to support your actual diagnosis may be either objective or subjective. Objective data is generally more important in forming the basis of your diagnosis. However, subjective data, especially regarding the patient’s pain level, can be important to both your diagnosis and overall care plan.
- For example, subjective data would be the patient saying they felt dizzy or confused. That subjective data can be quantified using objective data, such as that the patient’s blood pressure is 90/60 and their pulse is 110.
- Identify the problem that your nursing diagnosis will address. Look for patterns in the data you’ve collected. Various signs and symptoms may cluster together that point to the correct diagnosis.[7]
- Focus on the experience of the patient and those around them, not the medical diagnosis. A nursing diagnosis reflects the individual. No two nursing diagnoses will be alike, even for two patients diagnosed with the same condition.
- For example, let’s say your patient is diagnosed with a concussion. Your nursing diagnosis will include what your patient needs to help with this condition. It might include regular checks to make sure the patient stays awake. Ask questions like “what day is it?” and “where are you?”, to make sure the patient is oriented with time and place, and also watch for signs of confusion.
- Patients often will have more than one problem that needs to be addressed. Diagnose each problem separately.Tip: Whenever possible, verify your diagnosis with the patient, their family, or another nurse before beginning work on your treatment plan. For example, if you have a patient with a traumatic brain injury and you’ve diagnosed “chronic confusion,” you might talk to family and other nurses to confirm that the patient seems consistently confused and disoriented.
Part 2: Identifying Related Factors
- Look for the source of the patient’s problem. Once you’ve diagnosed the problem you’ll address from the nursing perspective, figure out why the patient is having that problem. This will help you decide what nursing interventions will work to alleviate the problem.[8]
- For example, suppose you’ve diagnosed chronic pain. The patient has a recent spinal cord injury. The spinal cord injury is most likely the cause or source of that pain.
- The patient’s medical diagnosis can provide some guidance here. For example, if you have a patient who was recently diagnosed with chronic obstructive pulmonary disease (COPD), that disease is most likely the source of your nursing diagnosis of a persistent cough.
- Keep in mind that patients may have more than one diagnosis. It’s best to rank them in order of severity to make it easier to address the patient’s needs. You may find them listed in order of concern on the doctor’s synopsis. It’s normal for the order to change over the course of treatment, so be mindful of the patient’s changing needs.
- Evaluate the patient’s history and overall health. Review the patient’s chart and records to determine factors related to their current condition. Lab reports and conversations with other health care team members may also be relevant.
- For example, if the patient is a chronic smoker, their smoking may be a related factor in their persistent cough or difficulty breathing.
- The patient and their loved ones can also offer you insight into the patient’s medical history and tell you about recent changes in behaviour.
- Include potential problems when determining related factors. Based on your knowledge of the patient’s condition, list symptoms or issues they might experience due to their current symptoms while undergoing treatment. Think of other symptoms or problems that tend to cluster together with the problems the patient has.
- For example, if you have a patient who has a persistent cough, sleep pattern disturbance related to the cough would be a potential problem related to the initial diagnosis. Anticipating these potential problems helps you customize treatment for the patient.
Part 3: Making Your Clinical Judgment
- Find the most appropriate nursing diagnosis. Look up the official terminology for the problem you observed. Use the NANDA-I and any other nursing textbooks you have to guide you. Write down the official terminology you find that best suits the needs and condition of the patient.[11]
- Once you have the nursing diagnosis, you can also look up potential outcomes and nursing interventions that are appropriate for your patient. Consider how each of these applies to this particular patient.
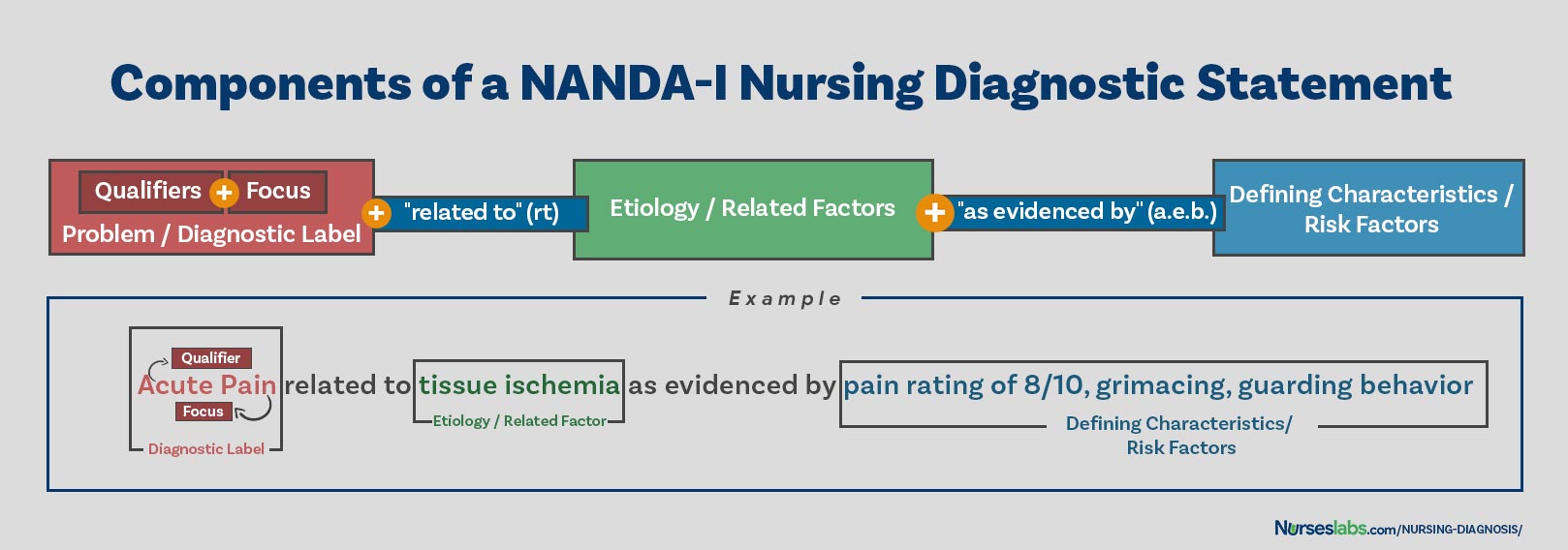
- Bring the related factors together for your diagnosis. The next part of your nursing diagnosis lists the related factors or causes of the patient’s problem. Look up the standardized terms for these factors in your textbooks, if you don’t already know them.[12]
- The related factors form the second part of your nursing diagnosis. After the specific diagnosis, write “related to” (also abbreviated “r/t”) or secondary to, followed by the list of sources or causes you’ve found for that problem.
- For example, suppose you have a patient with chronic confusion after a traumatic brain injury. You might write this up as “chronic confusion r/t possible traumatic brain injury” or “chronic confusion secondary to traumatic brain injury confirmed by MRI.”
- Make sure you work within the doctor’s diagnosis. If the diagnosis is not final, refer to the working diagnosis as “possible.”
- Summarize the data in an “AEB” statement. “AEB” is a common nursing abbreviation for “as evidenced by.” Sift through the data you’ve gathered to isolate characteristics that demonstrate the problem you’ve diagnosed.[13]
- Your textbooks will likely have lists of characteristics to look for that are related to a particular diagnosis. However, include only the characteristics that you have observed in this patient.
- Note whether the data is subjective or objective.
Nursing Diagnosis Examples
Chronic pain r/t spinal cord injury AEB patient’s statements, request for pain meds, inability to finish therapy without c/o pain.
Chronic confusion r/t traumatic brain injury AEB disorientation and cognitive dysfunction.
Conclusion
Nursing diagnosis is a process that gives you diagnostic criteria for presenting problems or the manifestation of the disease/condition that guide clinical judgements. Nursing diagnoses are written in a language to be understood by both professional nurse and patient, are expected to be able to be read by other caregivers, policy makers, researchers, managers, educators and other professions.