How to Write Prescription – Hello and welcome, here, you will find all you need to know about the prescription. There’s a ton of information out there, but trying to sift through it all can be time-consuming and frustrating. I’ve already done that for you, so all you have to do is check out the articles.
With the recent changes in optometric state laws, optometrists now have the privilege and responsibility for writing prescriptions. A written prescription is a legal document that should be prepared with care. While there are some variations from state to state, the prescription basically has 10 parts that will be discussed in this article. Use this information as a guide, but make sure you know the requirements in your own state. Also, be aware of the different requirements for prescriptions for controlled substances vs. noncontrolled substances.
Table of Contents
The Cost of Poor Prescription Writing
Poorly written prescriptions may be one of the main reasons there are so many medication errors today. Look at some of these commonly quoted statistics:
- Medication errors occur in approximately 1 in every 5 doses given in hospitals.
- One error occurs per patient per day.
- Approximately 1.3 million injuries and 7,000 deaths occur each year in the U.S. from medication-related errors.
- Drug-related morbidity and mortality are estimated to cost $177 billion in the U.S.
While these are just estimates from various studies and statistical models, the numbers are staggering. If there are 800,000 physicians in the United States, each physician accounts for $221,250! Do you still wonder why malpractice insurance is so expensive?Approximately 1.3 million injuries and 7,000 deaths occur each year in the U.S. from medication-related errors.Click To Tweet
Hopefully, if you are reading this, you’re interested in not making mistakes. Even though I don’t think I caused any major harm to any of my patients with prescription errors, I wish I had read something like this when I first started writing prescriptions in my 3rd year of medical school.
How to Write Prescription
Basic Information
- Include at least two patient identifiers. Patient identifiers are pieces of information used to clarify the identity of the patient. In all settings, you must include at least two of these identifiers.[1]
- Full name and date of birth are the two most common identifiers. For prescriptions fulfilled outside of a hospital, the patient’s phone number and/or current home address will usually be included, as well.
- One identifier isn’t enough, even if you use the patient’s full name. If two patients share the same name, it would be impossible to know which one the prescription refers to without any other identifier.
- Provide your information. As the prescriber, your name and contact information must also be listed on the prescription. Include your full name, the address of your medical practice, and the phone number of your medical practice.
- Note that your United States Drug Enforcement Administration (DEA) number must also be included somewhere on the prescription.
- In most cases, this information will already be printed on the prescription form. If it isn’t, however, you will need to write it manually.
- Note the date of the prescription. Some prescriptions must be filed within a certain time period. Even when the medication being prescribed does not fall into that category, you should still include the date.[2]
- Time-sensitive drugs are rated based on schedule categories.[3]
- Schedule I drugs have a high potential for abuse and have no legally accepted medical use within the United States.
- Schedule II drugs have a high potential for abuse but do have some legally accepted medical use.
- Schedule III drugs have some potential for abuse and can be used for some medical purposes.
- Schedule IV drugs have a relatively low potential for abuse and are legally permitted for some medical purposes.
- Schedule V drugs have an even lower potential for abuse and are legally permitted for certain medical purposes.
- Time-sensitive drugs are rated based on schedule categories.[3]
- Sign the prescription. You will need to sign each prescription before it can be considered valid. Your signature will usually go at the bottom of the form, regardless of whether or not there is a specific line for it there.
- It is strongly recommended that you write out the rest of the prescription and sign your name last. Doing so prevents unfinished or blank prescriptions from falling into the wrong hands.
Inscription
- Display the “Rx” symbol. “Rx” is the symbol for “superscription.” Write it just before you write out your instructions for the medication itself.
- On most prescription forms, the “Rx” is already printed.
- Write the inscription information immediately after this symbol. The inscription includes all of the information about the specific drug you want to prescribe.
- Write the medication. You should typically use the generic, non-proprietary name of the drug instead of the name brand.
- Use the name brand of the drug only when you specifically wish to prescribe the name brand. Keep in mind that doing so may make the prescription more expensive for the patient.
- If you want to prescribe the name brand, you should also include a note on the prescription reading “No Generics.” On most prescription forms, there will be a “Brand Name Only” or “No Generics” box you have the option of checking for this purpose.
- Mention the strength. Most medications come in multiple strengths, so you must mention the strength you wish to prescribe immediately after the name of the medication.
- The strength amount should be indicated in milligrams for tablets and suppositories and milliliters for fluids.
- Write words instead of abbreviations to avoid possible misunderstandings.
Subscription
- Include the prescription amount. Tell the pharmacist exactly how much of the medication should be filled and passed to the patient.
- This information should usually be preceded by an appropriate heading, such as “dispense,” “disp,” “#,” or “how much.”
- Include the specific bottle size or number of tablets/capsules. Spell the numbers out to avoid possible miscommunication.
- Note the number of permitted refills. For medications that treat a chronic condition or other similar reasons, you may wish to permit a certain number of refills before another prescription will be required.
- Only allow additional refills when the patient will need the exact same prescription multiple times.
- For example, you might wish to prescribe a year’s worth of oral contraceptives, yet each fulfillment of the prescription might only provide a month’s worth. On the prescription form, write “Refills 11” to indicate that eleven refills are permitted after the first fulfillment. After the final refill runs out, the patient will need a new prescription before any additional medication can be obtained.
- If you do not wish to permit any refills, write “Refills 0” or “Refills none” to indicate as much. Doing so reduces the risk of possible tampering.Advertisement
Patient Use Directions
- Specify the route. The route is the method used to take the medication prescribed. When writing the route, you can mention the instructions using either the accepted English term or the corresponding Latin abbreviation.
- Common options include:[7]
- By mouth (PO)
- Per rectum (PR)
- Intramuscular (IM)
- Intravenous (IV)
- Intradermal (ID)
- Intranasal (IN)
- Topical (TP)
- Sublingual (SL)
- Buccal (BUCC)
- Intraperitoneal (IP)
- Common options include:[7]
- State the dosage amount. State how much of the medication the patient should use each time he or she takes it. These instructions will be transferred to the prescription label once it is fulfilled.[8]
- For instance, you might write something like “one 30 milligram tablet” or “30 milliliters.
- Indicate the frequency. The frequency describes when and how often the medication should be taken. It is strongly recommended that you write out the frequency in full rather than using abbreviations.[9]
- In fact, a medication that must be used “daily” or “every other day” must be written out in full. Abbreviations for these frequencies are prohibited.
- Other frequency abbreviations can be used, but it is still recommended that you spell out the instructions instead of using the abbreviated form. Several common options include:
- Twice a day (BID)
- Three times a day (TID)
- Four times a day (QID)
- Every bedtime (QHS)
- Every four hours (Q4H)
- Every four to six hours (Q4-6H)
- Every week (QWK)
- Write when to discontinue use. Most medications must be taken until the drug runs out. In some cases, however, the patient should stop taking the medication once his or her symptoms disappear. You should specifically write which is the case on the prescription form.
- Consider including the diagnosis. When a medication should only be used on an “as needed” basis, you should include a brief diagnosis or reason for taking the medication.
- Specify this diagnosis with the abbreviation “PRN.” For example, the statement for a pain medication might read “PRN pain.”[10]
- Mention any other special instructions. Occasionally, there might be a special instruction that needs to go on the label. Let the pharmacist know to include it by specifically writing the instruction on the prescription form.
- A few common examples include:
- “Take with food”
- “Avoid alcohol”
- “Keep refrigerated”
- “Do not freeze”
- “For external use only”
- “Shake before instillation”
- A few common examples include:
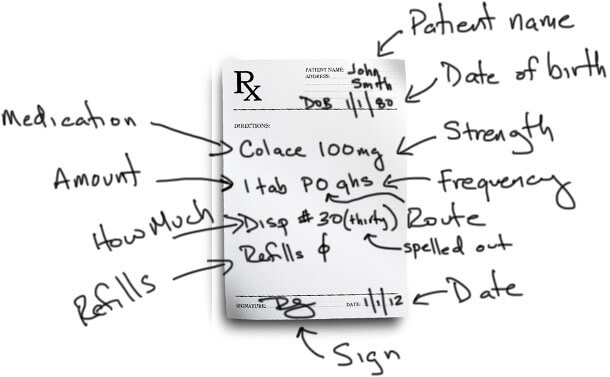
Breaking Down the Prescription Format
As I hinted above, here is the basic format of a prescription: First, we have the patient’s name and another patient identifier, usually the date of birth. Then we have the medication and strength, the amount to be taken, the route by which it is to be taken, and the frequency. For “as needed” medications, there is a symptom included for when it is to be taken.
The prescriber also writes how much should be given at the pharmacy and how many refills the patient can come back for. The prescription is completed with a signature and any other physician identifiers like NPI number or DEA number. Then the prescription is taken to the pharmacist who interprets what is written and prepares the medication for the patient. Now let’s look at each part of this individually.
Patient Identifiers
According to the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) national patient safety goals, at least two patient identifiers should be used in various clinical situations. While prescription writing is not specifically listed as one of these clinical situations, medication administration is. I think prescription writing should be in this category as well.Two patient identifiers should be included in a prescription to avoid medication errors.Click To Tweet
The two most common patient identifiers are their full name and date of birth. Patient identifiers are the first things to write on a prescription. This way you don’t write a signed prescription without a patient name on it that accidentally falls out of your white coat and onto the floor in the cafeteria.
Drug/Medication
This is an easy one. This is the medication you want to prescribe. It generally does not matter if you write the generic or the brand name here unless you specifically want to prescribe the brand name.
If you do want to prescribe the brand name only, you specifically need to indicate, “no generics.” There are several reasons you might want to do this, but we won’t get into that here. On the prescription pad, there is a small box which can be checked to indicate “brand name only” or “no generics.”If you only want to prescribe the brand name of a drug, you need to indicate ‘no generics’ on the prescription.Click To Tweet
Strength
After you write the medication name, you need to tell the pharmacist the desired strength. Many, if not most, medications come in multiple strengths. You need to write which one you want.
Often times, the exact strength you want is not available, so the pharmacist will substitute an appropriate alternative for you. For example, if you write prednisone (a corticosteroid) 50 mg, and the pharmacy only carries 10 mg tablets, the pharmacist will dispense the 10 mg tabs and adjust the amount the patient should take by a multiple of 5.
Amount
Using my previous example for prednisone, the original prescription was for 50 mg tabs. So you would have written, “prednisone 50 mg, one tab….” (I’ll leave out the rest until we get there). The “one tab” is the amount of the specific medication and strength to take.
Again using my previous example, due to the 50 mg tabs not being available, the instructions would be rewritten by the pharmacist as “prednisone 10 mg, five tabs….” You can see that “one tab” is now “five.” Pharmacists make these changes all the time, often without any input from the physician.
Route
Up until this point, we have been using plain English for the prescriptions. The route is the first opportunity we have to start using English or Latin abbreviations. Note: It is often suggested that to help reduce the number of medication errors, prescription writing should be 100% English, with no Latin abbreviations. I will show you both and let you decide.
There are several routes by which a medication can be taken. Some common ones are by Mouth (PO), per rectum (PR), sublingually (SL), intramuscularly (IM), intravenously (IV), and subcutaneously (SQ).It is often suggested that to help reduce the number of medication errors, prescription writing should be 100% English, with no Latin abbreviations.Click To Tweet
As you can see, the abbreviations are either from Latin roots like PO (“per os”) or just common combination of letters from the English word. Unfortunately, when you are in a hurry and scribbling these prescriptions, many of these abbreviations can look similar. For example, intranasal is often abbreviated “IN,” which, if you write sloppily, can be mistaken for “IM” or “IV.”
Common route abbreviations for prescription writing:
- PO (by mouth)
- PR (per rectum)
- IM (intramuscular)
- IV (intravenous)
- ID (intradermal)
- IN (intranasal)
- TP (topical)
- SL (sublingual)
- BUCC (buccal)
- IP (intraperitoneal)
Frequency
The frequency is simply how often you want the patient to take the medication. This can be anywhere from once a day, once a night, twice a day, or even once every other week. Many frequencies start with the letter “q.” This Q is from the Latin word quaque, which means once.
So in the past, if you wanted a medication to be taken once daily, you would write QD, for “once daily” (“d” is from “die,” the Latin word for day). However, to help reduce medication errors, QD and QOD (every other day) are on the JCAHO “do not use” list. So you need to write out “daily” or “every other day.”
Common frequencies abbreviations for prescription writing:
- daily (no abbreviation)
- every other day (no abbreviation)
- BID/b.i.d. (twice a day)
- TID/t.id. (three times a day)
- QID/q.i.d. (four times a day)
- QHS (every bedtime)
- Q4h (every 4 hours)
- Q4-6h (every 4 to 6 hours)
- QWK (every week)
The “Why” Portion
Many prescriptions that you write will be for “as needed” medications. This is known as “PRN,” from the Latin pro re nata, meaning “as circumstances may require.” For example, you may write for ibuprofen every 4 hours “as needed.”
What physicians and medical students commonly miss with PRN medications is the “reason.” Why would it be needed? You need to add this to the prescription. You should write “PRN headache” or “PRN pain,” so the patient knows when to take it.
How Much
The “how much” instruction tells the pharmacist how many pills should be dispensed, or how many bottles, or how many inhalers. Typically, you write the number after “Disp #.”
I highly recommend that you spell out the number after the # sign, even though this is not required. For example, I would write “Disp #30 (thirty).” This prevents someone from tampering with the prescription and adding an extra 0 after 30, turning 30 into 300.
Refills
The last instruction on the prescription informs the pharmacist how many times the patient can use the same exact prescription, i.e. how many refills they can get.
For example, let’s take refills for oral contraceptives for women. A physician may prescribe 1 pack of an oral contraceptive with 11 refills, which would last the patient a full year. This is convenient for both the patient and physician for any medications that will be used long term.
Conclusion
Though prescription is the name given to the formula for making medicines, especially for disease treatment, it is primarily referred to as directions or instructions issued by a medical practitioner. The prescription format consists of giving clear-cut direction about the drugs to be administered to the patients. Prescription writing need not be limited to medicines alone. It may also include other health care recommendations like physical therapies, dietician’s advice, lifestyle changes needed for better health etc.