How to Remove Hemorrhoids – A wide variety of treatment options exist forhemorrhoids, depending on the type ofhemorrhoid and the severity of your symptoms.
Avoiding constipation is often the key to treating hemorrhoids. And simple diet and lifestyle changes may help reduce hemorrhoid symptoms.
Eating a high-fiber diet can help make stools softer and easier to pass, reducing the urge to strain during bowel movements. Fiber is found in fruits, vegetables, whole grains, beans, nuts, and seeds.
The Academy of Nutrition and Dietetics recommends that adult women eat at least 25 grams of fiber each day, and that adult men eat at least 38 grams. (1)When adding fiber to your diet, go slow to avoid problems with excess gas.
If you’re having a hard time getting enough fiber in your diet, you can also take a fiber supplement.
Table of Contents
What Are Hemorrhoids?
Hemorrhoids are clumps of dilated (enlarged) blood vessels in the anus and lower rectum. The rectum is the last area of the large intestine before it exits to the anus. The anus is the end of the digestive tract where feces leaves the body.
Sometimes hemorrhoids swell when the veins enlarge and their walls become stretched, thin, and irritated by passing stool. Hemorrhoids are classified into two general categories:
- internal, originating in the rectum, and
- external, originating in the anus.
Hemorrhoids (also termed piles) have caused pain and irritation throughout human history. The word comes from Greek, “haimorrhoides,” meaning veins that are liable to discharge blood. If you’ve had a bout of hemorrhoid pain, you’re not alone. It’s estimated that three out of every four people will have hemorrhoids at some point in their lives. Even Napoleon suffered from hemorrhoids, which distracted him with severe pain during his defeat at Waterloo.
Enlarged Hemorrhoid Symptoms
Enlarged hemorrhoids are associated with symptoms such as
- itching,
- mucus discharge,
- burning at the anus,
- severe pain,
- a sensation that the bowel is not really empty, and
- bleeding without pain.
In this article, our medical experts will explain where hemorrhoid pain comes from, what hemorrhoids feel like, and how they are diagnosed. Then you will discover the various treatments for hemorrhoids both at home and at a hospital, along with the positive attributes and drawbacks of each hemorrhoid treatment.

Internal Hemorrhoids
Internal hemorrhoids sit in the inside lining of the rectum and are not obvious unless they are substantially enlarged, in which case they can be felt. Internal hemorrhoids are usually painless and become apparent because they cause rectal bleeding with a bowel movement.
Sometimes internal hemorrhoids prolapse or protrude outside the anus. If so, you may be able to see or feel them as moist pads of skin that are pinker than the surrounding area. These fallen hemorrhoids may hurt because the anus is dense with pain-sensing nerves. Such slipped hemorrhoids usually recede into the rectum on their own. If they don’t, they can be gently pushed back into place.

External Hemorrhoids
External hemorrhoids are located underneath the skin that surrounds the anus, and are lower than internal hemorrhoids. They can be felt when they swell, and may cause
- itching,
- pain, or
- bleeding with a bowel movement.
If an external hemorrhoid prolapses to the outside (usually in the course of passing a stool), you can see and feel it.
Blood clots sometimes form within this type of fallen hemorrhoid, which can cause an extremely painful condition called a thrombosis. If a hemorrhoid becomes thrombosed, it can look rather frightening, turning purple or blue, and could possibly bleed.
Despite their appearance, thrombosed hemorrhoids usually are not serious, though they can be very painful. They will resolve on their own in a couple of weeks. If the pain is unbearable, your doctor usually can remove the blood clot from the thrombosed hemorrhoid, which stops the pain.
Diagnosis
Your doctor might be able to see external hemorrhoids. Diagnosing internal hemorrhoids might include examination of your anal canal and rectum.
- Digital examination. Your doctor inserts a gloved, lubricated finger into your rectum. He or she feels for anything unusual, such as growths.
- Visual inspection. Because internal hemorrhoids are often too soft to be felt during a rectal exam, your doctor might examine the lower portion of your colon and rectum with an anoscope, proctoscope or sigmoidoscope.
Your doctor might want to examine your entire colon using colonoscopy if:
- Your signs and symptoms suggest you might have another digestive system disease
- You have risk factors for colorectal cancer
- You are middle-aged and haven’t had a recent colonoscopy
Treatment
Home remedies
You can often relieve the mild pain, swelling and inflammation of hemorrhoids with home treatments.
- Eat high-fiber foods. Eat more fruits, vegetables and whole grains. Doing so softens the stool and increases its bulk, which will help you avoid the straining that can worsen symptoms from existing hemorrhoids. Add fiber to your diet slowly to avoid problems with gas.
- Use topical treatments. Apply an over-the-counter hemorrhoid cream or suppository containing hydrocortisone, or use pads containing witch hazel or a numbing agent.
- Soak regularly in a warm bath or sitz bath. Soak your anal area in plain warm water for 10 to 15 minutes two to three times a day. A sitz bath fits over the toilet.
- Take oral pain relievers. You can use acetaminophen (Tylenol, others), aspirin or ibuprofen (Advil, Motrin IB, others) temporarily to help relieve your discomfort.
With these treatments, hemorrhoid symptoms often go away within a week. See your doctor in a week if you don’t get relief, or sooner if you have severe pain or bleeding.
Medications
If your hemorrhoids produce only mild discomfort, your doctor might suggest over-the-counter creams, ointments, suppositories or pads. These products contain ingredients such as witch hazel, or hydrocortisone and lidocaine, which can temporarily relieve pain and itching.
Don’t use an over-the-counter steroid cream for more than a week unless directed by your doctor because it can thin your skin.
External hemorrhoid thrombectomy
If a painful blood clot (thrombosis) has formed within an external hemorrhoid, your doctor can remove the hemorrhoid, which can provide prompt relief. This procedure, done under local anesthesia, is most effective if done within 72 hours of developing a clot.
Minimally invasive procedures
For persistent bleeding or painful hemorrhoids, your doctor might recommend one of the other minimally invasive procedures available. These treatments can be done in your doctor’s office or other outpatient setting and don’t usually require anesthesia.
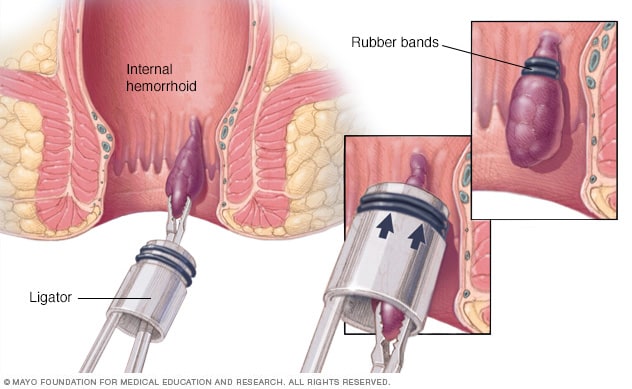
- Rubber band ligation. Your doctor places one or two tiny rubber bands around the base of an internal hemorrhoid to cut off its circulation. The hemorrhoid withers and falls off within a week. Hemorrhoid banding can be uncomfortable and cause bleeding, which might begin two to four days after the procedure but is rarely severe. Occasionally, more-serious complications can occur.
- Injection (sclerotherapy). Your doctor injects a chemical solution into the hemorrhoid tissue to shrink it. While the injection causes little or no pain, it might be less effective than rubber band ligation.
- Coagulation (infrared, laser or bipolar). Coagulation techniques use laser or infrared light or heat. They cause small, bleeding internal hemorrhoids to harden and shrivel. Coagulation has few side effects and usually causes little discomfort.
Surgical procedures
Only a small percentage of people with hemorrhoids require surgery. However, if other procedures haven’t been successful or you have large hemorrhoids, your doctor might recommend one of the following:
- Hemorrhoid removal (hemorrhoidectomy). Choosing one of various techniques, your surgeon removes excessive tissue that causes bleeding. The surgery can be done with local anesthesia combined with sedation, spinal anesthesia or general anesthesia. Hemorrhoidectomy is the most effective and complete way to treat severe or recurring hemorrhoids. Complications can include temporary difficulty emptying your bladder, which can result in urinary tract infections. This complication occurs mainly after spinal anesthesia. Most people have some pain after the procedure, which medications can relieve. Soaking in a warm bath also might help.
- Hemorrhoid stapling. This procedure, called stapled hemorrhoidopexy, blocks blood flow to hemorrhoidal tissue. It is typically used only for internal hemorrhoids. Stapling generally involves less pain than hemorrhoidectomy and allows for earlier return to regular activities. Compared with hemorrhoidectomy, however, stapling has been associated with a greater risk of recurrence and rectal prolapse, in which part of the rectum protrudes from the anus. Complications can also include bleeding, urinary retention and pain, as well as, rarely, a life-threatening blood infection (sepsis). Talk with your doctor about the best option for you.
Hemorrhoid Treatments in Your Doctor’s Office
If you have hemorrhoids and at-home treatments to shrink them or ease the pain haven’t worked, your doctor may be able to help.
Several procedures can be done in a doctor’s office, and each has advantages and disadvantages.
Rubber-Band Ligation (Banding)
Your doctor will take a tiny rubber band (only a few millimeters wide) and put it over the base of an internal hemorrhoid to cut off the flow of blood. The hemorrhoid usually shrinks and falls off (along with the band) in about a week.
If you have several hemorrhoids, you may need to have this done every few weeks. This treatment can be painful and cause bleeding. More rarely, it also may cause blood clots or infections.
Hemorrhoids treated this way are less likely to come back than with other treatments.
Sclerotherapy
Your doctor will give you a shot that puts chemicals into the hemorrhoid tissue. These chemicals also cut off blood flow to the hemorrhoids and shrink them. You may need to have this done every few weeks until they go away completely.
You may feel mild pain or pressure after, but infections are rare. With this treatment, the hemorrhoids often come back in a few years.
Infrared Coagulation
With this treatment, your doctor focuses an infrared light on a hemorrhoid, and the heat causes scar tissue to form and blood flow to the hemorrhoid to be cut off.
Generally, coagulation treatments have few side effects and cause very little pain. However, hemorrhoids are more likely to come back with these treatments than with banding.
Electrocoagulation
This is similar to infrared coagulation, except instead of an infrared light, your doctor uses heat from an electric current to create scar tissue and cut off the hemorrhoid’s blood supply.
Hemorrhoidal Artery Ligation and Recto Anal Repair (HAL-RAR)
Hemorrhoidal Artery Ligation and Recto Anal Repair (HAL-RAR) is a new procedure in which a miniature Doppler sensor is inserted in the anus to detect the arteries supplying blood to hemorrhoids. The surgeon can pinpoint the arteries supplying the hemorrhoids and can tie them off to cut the blood supply. The hemorrhoids are reduced almost immediately and within weeks, are no longer noticeable. The procedure is effective and virtually painless, but it is not simple.
Conclusion
The best way to prevent hemorrhoids is to keep your stools soft so they are easy to pass and don’t require straining. Eating a high-fiber diet and drinking plenty of fluids (six to eight glasses each day) can help you stay regular and keep your stools soft, and may reduce constipation and the need to strain on the toilet, lowering your risk of developing new hemorrhoids.